Transfusion-dependent beta (β)-thalassemia (TDT)
is the most severe form of beta-thalassemia1
Transfusion-dependent beta (β)-thalassemia (TDT) is the most severe form of beta-thalassemia1
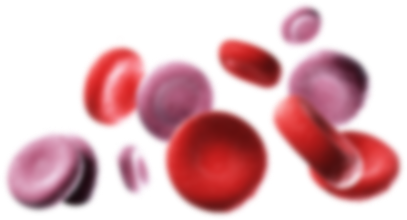
TDT is characterized by reduced or absent production of functional beta-globin, which is essential for forming adult hemoglobin. To survive, patients living with TDT require regular lifelong red blood cell transfusions, but this only temporarily addresses the symptoms of disease.1,2 It’s time to challenge our understanding of TDT and consider its genetic cause.
TDT is characterized by reduced or absent production of functional beta-globin, which is essential for forming adult hemoglobin. To survive, patients living with TDT require regular lifelong red blood cell transfusions, but this only temporarily addresses the symptoms of disease.1,2 It’s time to challenge our understanding of TDT and consider its genetic cause.